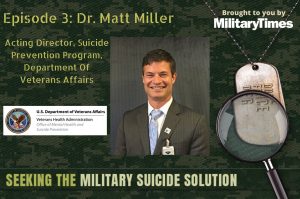
About Today’s Guest:
Dr. Matt Miller is currently the Acting Director for Suicide Prevention, Office of Mental Health and Suicide Prevention for the Department of Veterans Affairs. He was appointed the permanent Director of the Veterans Crisis Line on July 23, 2017. Dr. Miller joined the VA in January of 2012 as the Chief of Mental Health at the Saginaw VAMC in Saginaw, Michigan. He has been detailed to the national mental health office as a Technical Assistance Specialist and as Senior Consultant for National Mental Health Technical Assistance. Before coming to VCL, Dr. Miller served as Deputy Chief of Staff for the Saginaw VAMC, with responsibility and oversight of facility-wide access and quality, assisting Saginaw with achieving and maintaining a 5-star ranking by facility complexity in the nation on SAIL. Within his role as Director of the VCL, Dr. Miller has been privileged to be a part of a team that has created and implemented a third call center in Topeka, KS, has increased total staffing to 900+ FTE becoming the world’s largest crisis call center, has achieved a 96 percent reduction in Rollover calls to the backup call center, has developed an industry-leading Quality and Training program, has achieved certification via nationally-recognized oversight organizations, and has innovated cutting edge research projects in the field of suicide prevention.
Dr. Miller received his PhD from Michigan State University, East Lansing, and his MPH from the University of Michigan, Ann Arbor. He completed a professional clinical psychology internship via the United States Air Force (USAF), Wright Patterson Medical Center, Wright Patterson Air Force Base, Ohio. Thereafter, he was assigned to Vance Air Force Base in Enid, Oklahoma, as Chief of Mental Health. Miller was awarded “Officer of the Year” representing the 71st Medical Group in 2003; in the same year, he was awarded the USAF “Cutting Edge Award” for program development and outcomes addressing and treating Complicated Airsickness Management for Pilots.”
Links Mentioned in this Episode:
Episode Sponsor:
Shauna’s latest book: Beyond the Military: A Leader’s Handbook for Warrior Reintegration
Duane’s latest book: Military in the Rear View Mirror: Mental Health and Wellness in Post-Military Life
Using an app makes subscribing and listening to podcasts (both ours and others) so much simpler. Just subscribe to Seeking the Military Suicide Solutionwithin your app and it will automatically update every time a new episode is released. You can also find all of the podcast players here.
Episode Transcript:
Duane France: (00:00) Welcome to episode three of the Seeking the Military Suicide Solution Podcast brought to you by the military times. I’m Duane France.
Shauna Springer: (00:07) and I’m doc Shauna Springer.
Duane France: (00:09) and we’d like to thank you for taking the time to learn more about suicide in the military affiliated population. I’d also like to thank our sponsors, milMedia group. Milmedia group is a proven web design and digital media agency specializing in supporting organizations focusing on the military population. Find out more about them at milmediagroup.com
Duane France: (00:38) Thanks again to everybody for joining us to listen to an honest conversation about service member veteran and military family suicide. The response to the concept of the show has been outstanding. It’s generating a lot of conversation and that’s what we’re trying to do. Our guest today is Dr. Matt Miller, Acting Director for Suicide Prevention for the Department of Veterans Affairs. Shauna?
Shauna Springer: (01:00) Today we’re pleased to bring Matt Miller onto the show. As Duane said, his official role as Acting Director for Suicide Prevention for the Department of Veterans Affairs, but like other guests, this is not a job. It’s personal. The back story is this: many years ago, Matt Miller was the only psychologist on Vance air force base in Enid, Oklahoma. In this role, he was in charge of mental health for the entire base. He led all efforts related to suicide prevention, family advocacy, substance abuse treatment, and critical incident response services. He also became part of the inner circle of major John Ruocco. By all accounts, John was the kind of guy that lit up a room, a decorated Cobra pilot. He was someone who had more than 75 combat missions under his belt and John was a rock for many people, including Matt Miller. John was also someone that never fully revealed the depth of his hidden pain, even to those who love him most. When John died by suicide in February, 2005 the grief that initially engulfed those closest to him later fueled an explosion of posttraumatic growth. John’s wife, Kim Ruocco, who will be featured on a future episode of Seeking the Military Suicide Solution, has led efforts to develop and refine what is now the leading postvention model in the country. And Matt Miller went on to become the director of the veteran’s crisis line and is now the acting national director for suicide prevention for the department of veterans affairs.
Duane France: (02:32) Yeah, it’s really great to hear Matt’s background and like we’ve talked about even in the introductory episode, you know, the reasons why people come to this work are often very personal and that’s definitely the way it was with Matt. So let’s get into the conversation and we’ll come back afterwards to pull out some of the key points.
Duane France: (03:01) The work that you’re doing now and the work that you’ve done before focusing on suicide in the veteran population with the VA. What do we know that works with preventing suicide in the veteran population?
Dr. Matt Miller: (03:16) Hmm. We know…that’s a question that we all are constantly asking in the context of such an important issue where lives are truly on the line on a daily basis. In terms of what we know works. We know that a public health approach to suicide prevention is evidence-based and work. A public health approach means that…kinda consider it like an equation, where you have an equal sign and on the right hand side of the equal sign you have public health approach. So really then what’s on the left hand side of the equal sign, there’s two things. Number one, there’s clinically based interventions and then number two, there’s community based intervention. And they, those two clinically based interventions and community based interventions are joined by a plus sign. So clinically based interventions plus community based interventions equals a true public health approach.
Dr. Matt Miller: (04:33) If you altered the left hand side of that equation and were to say, for example, clinical clinically based interventions minus community based interventions, you would not have public health approach on the other side of the equal sign. If you were to remove the equation and simplify it, let’s say, and simply put that clinically based interventions equal a public health approach or community based interventions equal a public health approach, you would not have a true public health approach. So what we’re learning works the direction that we’re learning and verifying that we need to head with the critically important issue of suicide prevention is the clinically based interventions plus the community based interventions together and within a integrated plan, strategy, and delivery system such as the VA. Now in terms of what works and what we’re seeing here within each of those two important components…
Dr. Matt Miller: (05:57) Our 2019 annual suicide prevention report provides some insight, for example, under a clinically based intervention we see from the 2019 report based upon 2017 data that there has been a decrease in the suicide rate for veterans diagnosed with a depressive disorder and receiving VHA care. I asked the team if they could convert that rate of decrease into a calculated figure for lives saved from the 2016 data to this 2017 data based upon the rate decrease. So they came back to me and they said, Matt, this translates to 87 lives saved from 2016 to 2017 of individuals, veterans, diagnosed with depression and in VHA care. 87 lives saved. That’s significant. That tells us that evidence based care can be effective and is effective and can save 87 lives if not more when implemented in evidence-based manner. .
Dr. Matt Miller: (07:20) So that’s an anchor of hope that we hang on to and as a data point in terms of that, which is a fact of. We also know that if you take a look, it gets a little mathy, but if you take a look at the slope of increase for suicide among veterans and you were to compare the slope, the increase, for veterans in VHA care versus veterans, not in VHA care, the slope, the rise is significantly different between veterans in VHA care and veterans, not in VHA care. And it’s much lower for veterans in VHA care versus not. Specifically, there’s about a 1% slope rise, if you will, for veterans in VHA care compared to over 11% for veterans not in VHA care. So all of this to say, Duane, and all of this to get back to the point that under the heading of clinically based interventions, we know that there are things that work that we continue then to press forward with and find new ways to implement now in 2019 going into 2020 under the clinically based interventions heading
Dr. Matt Miller: (08:33) Under the community based intervention setting. We know from our clinic practice guidelines issued by the VA and DOD and a national leading collaborative effort that lethal means safety is a very effective tool on the population, community based level for suicide prevention. So that’s something that we look to move forward and have developed a toolkit for safe firearm storage in the community that represents a partnership between us, the American Foundation for Suicide Prevention and the National Shooting Sports Foundation. So there’s a couple of specific points, I think, in reference to your very good question,
Duane France: (09:27) You know, I really appreciate that visualization because I’m thinking about other public health dilemmas and how that would translate. So when it comes to smoking cessation, nobody doubts whether or not there is a clinical approach, a medical approach really. But a clinical approach plus a community approach. Let’s say with a reduced drunk driving that’s not necessarily a medical thing. And so it’s not really a clinical approach required. But the unique aspect of suicide because it’s psychological and it impacts the community, the two things are combined and so it’s much more in line with something like smoking cessation or reducing obesity or heart risks cardiac risk.
Dr. Matt Miller: (10:16) Yeah, there’s parallels there. But let’s even go back. Let’s go back to the driving while intoxicated example that you nicely cited. We can take a look at that across community and clinical. So on the community based intervention levels, you can have very effective public messaging campaigns that highlight the impact of driving while intoxicated on the individual’s lives and on the community as a whole. And, and everyone listening right now can think probably and see some of those images from those campaigns. On the clinical side, you can think, well, there may be individuals who have a substance use disorder and they would benefit from evidence-based alcohol addiction, alcohol dependence or alcohol abuse treatment. And as they engage in that treatment, yes, it will positively impact that which we’re doing more broadly with regard to decreasing driving while intoxicated incidents and impact. But if you were to just rely on the clinically based interventions to address this, you wouldn’t impossibly cover the entire spectrum that you need because every situation doesn’t necessarily entail alcohol dependence or an alcohol abuse disorder. Sometimes it does and therefore it’s important to have that treatment available and evidence based. But it also involves a community approach of messaging to everyone in the community, whether you may be working through an alcohol use or abuse problem or not.
Duane France: (12:15) After the break, Matt and I talk about why the public health approach to suicide is different than the public health approach to things like DUIs or heart disease.
milMediaGroup: (12:37) Hi, I’m Alyssa Mosher. I’m a local army spouse, daughter, sister and a proud team member of milMedia. I’m here at our headquarters at the great Fort Hood, Texas. MilMedia is a military affiliated team that wants to serve you the way that you served our country. With mostly military retirees, veterans and families as our staff, we understand the military mindset. milMedia is the one place that prioritizes your goals above all else, which you will see from our incredible customer service. With over 25 years of experience, we work with everyone from startups, small businesses, entrepreneurs and nonprofits. milMedia group is the digital division of Top Sarge Business Solutions that specializes as a web design and digital marketing platform. So visit our website today for a free website analysis so that you can sit back, relax, and let us give you the perfect online presence to hear more about what milMedia is doing and will continue to do, call me today at (254) 554-0974 or visit our website. That’s milMediagroup.com So call me whenever you’re ready.
Duane France: (13:46) That puts me in mind, perhaps the question, and maybe we won’t answer it in this short of time, but why is it different than when it comes to suicide? Because in the community, the minute somebody says suicide, it becomes something for the experts to do. It’s not something for the barista or the mechanic or the plumber,
Dr. Matt Miller: (14:02) Which is exactly, exactly, Duane, what we’re trying to change. If you take a look at our Be There campaign and you take a look at what we talked about extensively during the month of September and suicide prevention month, you just hit the nail on the head on our theme. Our theme under Be There was everyone has a role to play with suicide prevention. A good example of this I think is some work being done by a colleague of ours out in Oregon. And what they found at the local community level when they really dove into some things regarding what’s happening with suicide in our community, they found the last 24 to 48 hours of individual’s lives prior to suicide. They commonly in that area visited animal shelters and hotels. And you say, well, why animal shelters? Well, they were arranging plans and care for their beloved pets.
Dr. Matt Miller: (15:09) Why hotels? They were often going there as a location so that they weren’t in a home setting, impacting their family or loved ones in a more perceived adverse way. So based upon that data, a team deployed training and gatekeeper training for suicide prevention at animal shelters locally and at local hotels, teaching individuals in those settings, individuals on the front lines, they’re not clinical psychologists, they’re not primary care physicians. They’re good people working at animal shelters in hotels, teaching them how to recognize warning signs, teaching them what to do when they recognize these warning signs and then engaging based upon that information. It’s one of the few counties in our nation that’s actually seen a decrease in suicide. So that gets to the point and reinforces exactly what we’re trying to accomplish with Be There. Now, some may say, Matt, you’re abdicating your responsibility here. You’re trying to put suicide prevention on the front line individuals while people like you aren’t doing what they need to do.
Dr. Matt Miller: (16:30) I say, I agree. That’s why we have, and that’s the importance of the additive model of the public health approach. It’s important that you do have those clinically based interventions available and access to those clinically based interventions. But you know what, although there’s a relationship between depression and suicide, there’s not always a relationship between suicide and depression. So you need to be able to have the clinically based interventions that address depression, that address substance use disorder that address relationship problems and issues. But you also need to have the community based intervention approach where all of us are looking out for each other and all of us are ready to engage. When we see something.
Dr. Matt Miller: (17:27) Duane, I give an example, a personal example of this from my own life. It’s a little bit of an apples to oranges comparison, but I’ll share it. I often tell of a time where I have my four daughters and we were out for dinner and we were at a restaurant, it was called Smoking Charlie’s at the time. And we were sitting there and all of a sudden I heard some coughing over my shoulder behind me. And one of my daughters who was sitting across from me said, daddy, is that guy choking? I turned around and I looked, and there was a man standing at his table and he had all the hallmark signals and signs of choking. He was coughing, he was holding and grasping his throat. He was leaning over, he had the look of desperation on his face. And I, my first thought was, I hope someone does something about that.
Dr. Matt Miller: (18:28) And my second thought was, Matt, you could do something. You could do the Heimlich. And then my next thought was, what if I screw it up? What if I don’t do it right? What if I don’t help? And so this time that I was thinking and churning on these issues, someone stood up, someone administered the Heimlich maneuver on this individual and they dislodged the potato chip that this individual was choking on and this individual lived. I stepped back from that, as ashamed I am of that example. I think it provides an illustration of the role we can all play. I don’t need to be a cardiologist, I don’t need to be a pulmonologist to administer the Heimlich maneuver for someone at Smoking Charlie’s who’s choking on a potato chip. I can be the person beside them that simply engages the Heimlich maneuver and saves a life. And in that same way, the community and everyone therein has a role to play with, “See something, do something.” Yeah. Do we not need pulmonologists? Do we not need cardiologists? Do we not need EMS to show up and still do a followup check to make sure the individuals, okay? Yes! We need all of that. So that illustrates the community plus the clinical coming together in a lifesaving daily way,
Duane France: (19:53) You know, so that…and obviously the thing that works is the connection between the community and clinically based practices, again, needing both of those to balance the equation. And that’s also illustrating the gap that occurs because we don’t have that connection. We as clinicians…and I’m saying it often on the show and I’m gonna say it often in my community, if we had the solution then the problem would be solved by now, but we’re not the first one in contact, right? The, the EMS was not the first person that come in contact the gentleman in the restaurant. You know, so that illustrates both what’s working and and the gap and even, you know, maybe what actions people can take is to, you know, learn and be educated on the signs and symptoms. But for listeners, what’s not working, right? There’s something that people, you know, think that is effective or is working, that’s not working when it comes to preventing suicide.
Dr. Matt Miller: (20:50) Hmm. Oh, I think what’s not working is a over-reliance on, to the exclusion of the other, an over-reliance on clinically based interventions to the exclusion of community based interventions and conversely and over-reliance on community based interventions to the exclusion of continuing to attend to that which we can do and furthering clinically based intervention. What’s also not working is when there’s no plus sign between the clinically based and the community based. As you said, they’re not talking or coordinating together. There’s a gap, there’s no plus sign unifying them. That scenario is going to get us to, is going to keep us at a point where suicide prevention then as a whole is not working for our nation. And we see that historically. Suicide is not a veteran specific issue. It is an issue that impacts veterans in a meaningful way. It is an issue that we must continue to find ways to turn around and address but it occurs within a larger context of our United States population. Our brothers and sisters, wherein suicide is on a rise across our nation as a whole. It’s been rising since 1999. It’s the 10th leading cause of death in adults, but it’s become the second leading cause of death in individuals age 10 to 22. So this is a broader issue that merits a national level discussion and the VA can lead the way within that in terms of veterans, veteran care and that which we’re doing to unify the clinical and the community.
Duane France: (22:48) Oh, I absolutely agree. I think one of the things that I’ve often said is you know, as veterans go, so go our nation not that veterans need to be taken care of, but you know, it is a microcosm, but if we can figure out how to address veteran homelessness, then we can apply those techniques to homelessness in the community. But with the veteran population, essentially it can be a test bed, but that’s what you’re talking about is if we can help solve this corner of what the issue is, then that’s going to impact the issue overall.
Dr. Matt Miller: (23:19) Yes. Yeah. In some ways we are the canary and we are going into places here that are dark that no one has been. And we are testing things here in the name of saving lives. Someone’s got to do it. And I’m proud to be a part of the VA team on a community that is doing this.
Duane France: (23:43) Yes. And I absolutely agree and I thank you and your team. There’s a lot of great work coming out of the office of suicide prevention. Like you said, your, your lethal means safety work especially between AFSP and the National Sports Shooting Foundation. Great stuff. And, and I really think that we’re at a point where it’s going to start having more momentum. I really appreciate you coming on the show today, Matt.
Dr. Matt Miller: (24:13) You know, safe messaging and talking about suicide in a way that doesn’t create fear, that doesn’t promote stigma but instead promotes awareness and promotes constructive engagement. That’s a big part of the battle here. And what you’re doing today, is being a frontline troop in that battle. You’re opening up the discussion, you’re de stigmatizing, you’re offering suggestions for converting awareness into engagement. So the thanks are due to you, not to me. And to your audience,
Duane France: (24:48) That is a, that’s definitely the goal.
Duane France: (24:59) So I had a really great time with that conversation. Matt is somebody, again, we’re really working through the beginning of these shows, the list of people that I really wanted to come on and sort of set the tone of suicide prevention. And when we think about suicide prevention in the veteran military family population, of course we think about the Department of Veterans Affairs not just because of the size of it, but because of the work that’s been done to the research and the interventions. And so it was great to be able to have Matt come on the show to talk about some of the things that the VA is doing when it comes to veteran suicide specifically. So Shauna, what did you think about the show?
Shauna Springer: (25:42) Yeah, I thought there were some real important insights in there. One of the important insights that stood out to me was the insight about hotels and animal shelters. I sometimes think that important insights are overlooked and are so clear in retrospect. When he talked about community level efforts and how these efforts have led to insights around high risk indicators, this felt really important to me. So specifically when he talked about how people in the suicidal mind-state often visit animal shelters and hotels before they attempt to end their lives. Now this makes total sense. I’d be willing to bet that, you know, what I say is also true for you, Duane. In my years as a frontline provider, I’ve had many patients tell me that the only thing keeping them alive is that they wouldn’t abandon a beloved pet. So, you know, it makes sense that people are trying to ensure that their pets are not abandoned before they consider attempting suicide. It also makes sense that visits to hotels would be paired with attempts since people often want to create distance with their loved ones who might find them just after the death. So by identifying these patterns and helping staff members of animal shelters and hotels be vigilant for people who may be in distress, we may be able to prevent perfect storms from ending in lasting tragedy. And this was really exciting to hear since this kind of very practical insight is why I wanted to do this podcast with you. What did you think?
Duane France: (27:16) Yeah, I agree. And definitely that idea of, you know, suicide hotspots. Some people think about suicide hotspots as locations where people often attempt to take their life like the Golden Gate Bridge or a particular rail crossing or bridge in someone’s community. But we’re getting to the point and, and I’m speaking definitely here in Colorado where most communities should get to the point of, you know, the corner knows the zip codes and even to the addresses of when these these deaths by suicide and just like anything else, if you have a larger cluster of suicides in one particular area, then it would be very good to concentrate efforts in that area. And it would be different between communities. It may be hotels in Oregon. Or it may be parking lots in, you know, North Dakota, right? I mean,, it could be something different in each community. But yeah, I absolutely believe the concept is something that is intriguing and to be honest, something that we’re looking to implement in our community to see where the majority of our suicides are clustered.
Shauna Springer: (28:29) Right. It’s, you know, really understanding that concentration of where people are going to travel before they consider making an attempt. I think that’s going to help us with the public health approach because it will help us understand who we need to really equip.
Duane France: (28:46) Yeah. You know, and I think that’s equipping people who may not think they need to be equipped or it’s not even a concept for them. Another thing that we have, in our community efforts here, the restaurant and bar association has reached out to our local organization saying, can you teach us suicide prevention? So who, but the bartenders, right? The bartender is the late night therapist kind of thing. But they reached out and said, can you give us help? So it is giving people those tools that they may not even realize they need or really aren’t comfortable using. Anything else you got from Matt’s conversation?
Shauna Springer: (29:29) Yeah. You know, speaking of restaurants, I really appreciated the personal example that Matt shared of being in the restaurant, seeing someone choking and having the immediate thought, gee, I hope somebody helps that guy. I think this is such an important point. So much of the time I think we don’t intervene in situations, not because we don’t care if someone lives or dies, but because we’re fearful that we’ll screw it up or we think we’re not qualified to assist. And this kind of made me reflect on bravery. A few thoughts I wanted to share. Bravery is something that can be domain specific. For example, I’ve worked with a number of combat veterans who would walk into the kill zone of an ambush without flinching. They’re terrified to tell their partners that they love them and they need them.
Shauna Springer: (30:15) And I’ve worked them through this barrier. So I know that the instinct to avoid can be overcome if someone gives it a real focused effort. Also bravery can be developed. I think through practice. For example, many people who serve in the military are initially fearful or uncomfortable about using firearms or using violence against other people. But military training helps these people overcome that avoidance instinct. And some of them become our finest soldiers and Marines and operators because they have a level of humility and restraint that others never had to begin with. So my thought is that for the public approach to suicide to really work, we have to figure out a way to overcome our initial avoidance instinct. We need to trust our gut when it calls to us and we need to move in close when we sense that someone is in a dark and hopeless place. I think this kind of bravery can absolutely be learned.
Duane France: (31:07) You know, this is actually something that I often brought up when I was doing the applied intervention skills training. And I’d asked the attendees, you know would you do anything to save the life of a fellow veteran, you know, well, yeah, of course I would, right? You know, run into a burning building. And they would say, yes. And I said, what if that includes looking them in the eye and asking them, “are you thinking of killing yourself?” And then people are like, “Oh I don’t know about all that.” Well and yes, bravery is bravery but are we willing to, and this and that was one of my things and that’s what in things like assist and QPR and these trainings do for you is to get you used to asking those questions and just like basic training and I like that analogy but doing stressful things in non stressful situations so that you can then do those things in stressful situaitons.
Shauna Springer: (31:59) Exactly. Exactly where my mind goes to, that there’s a way to habituate to being uncomfortable because it’s a different domain of bravery, you know to go into a burning building or to look someone straight in the eye in the context of a relationship that’s trusting and intimate in the sense of loving someone as a brother or sister and saying, are you thinking about having thoughts of ending your life right now. And holding the gaze. It’s hard for people to look at each other full in the face and not ask anything even harder for them to ask about life or death matters. But we need to be doing that for a public health approach to work.
Duane France: (32:39) Yeah. And I think, again, there’s that idea of what maybe came out in that first episode with Dr. van Dalen was suicide prevention is not something we do to someone. It’s something we do with people, right? It’s a mutual thing that we do with someone who happens to be in crisis. And that does impart a responsibility on both sides, I think. But it’s a matter of a partnership. Whereas, you know, doing the Heimlich maneuver as Matt had described, that’s something you do to somebody, right? You do CPR to somebody. You don’t do CPR with somebody. But this is a very highly relational situation where we have to do this with each other.
Shauna Springer: (33:19) Exactly. Yep. Fully agree.
Duane France: (33:22) Yeah. I really appreciated Matt’s conversation and the opportunity to, and even their willingness, the VA’s willingness to come on the show and have this conversation in a very public way to be able to make a difference. So I’m really excited about how this episode will be received.
Shauna Springer: (33:43) Yeah, I think there’s a lot of confusion and misunderstanding about the people behind the roles. And one of the things that was neat about this episode is to really understand where Matt is coming from and this is personal for him. And so it’s not just a role in a job.
Duane France: (33:59) Absolutely. So everybody makes sure to continue to stay tuned to listen to more episodes about seeking the military suicide solution. Make sure to check the show notes at www.veteranmentalhealth.com/stmss03, where you can get links to all the things that Matt talked about in the episode. And you can also find the shows on military times.com. While you’re at it, check out our sponsors milMedia group. They’re a web design and digital media agency with over 25 years of experience in supporting service members, veterans and their families. They specialize in working with startups, small businesses, entrepreneurs, nonprofits and city, state and local governments. As a veteran owned business, they’re uniquely qualified to work with those that want to reach an audience in the military and veteran space. Do you have a dream or a vision they can help you bring it to life and get it in front of your audience? You can contact them at (254) 554-0974 or find them online at www.milmediagroup.com
Shauna Springer: (34:56) Just a reminder that the guests and reflections on this show are for informational purposes only and should not be considered professional advice. While Duane and I are mental health professionals, we are not your mental health professionals. We always recommend that you discuss these things with a licensed clinician.
Duane France: (35:12) You can find out more about the work that Shawna’s doing by checking out her latest book, Beyond the Military, a Leader’s Handbook for Warrior Reintegration, and the work that I’m doing with my latest book, Military in the Rear View Mirror. Both are available on Amazon and we’ll have links to those in the show notes.
Duane France: (35:27) and always remember, you can connect with the veteran crisis line by calling (800) 273-8255 and pressing one, chat online with them at veterancrisisline.net or texting, 838255. Thanks again for joining us to talk about Seeking the Military Suicide Solution and make sure to follow Military Times on social media to keep up with the latest shows. Join us next time for another great episode and until then, remember, you’re not alone. Ever.